Pancreatic islet cell transplantation is a novel treatment option that is in the approval process for patients with diabetes. Doctors get islet cells (cells from the pancreas which make and release insulin) from a deceased donor and transplant them into the patient. The transplant process involves a minor procedure in which doctors make a small cut in the patient’s upper abdomen and inject the healthy islet cells into the patient’s liver. Once the transplant has been completed, the newly injected islet cells begin to make and release insulin almost right away however, the patient will still need insulin for up two weeks after the transplantation to make sure the islet cells can work completely on their own. Additionally, patients that have recently received an islet cell transplant are also required to take medications called immunosuppressants. These medications help to stop the body from rejecting the new islet cells in their liver. Rejection occurs when the body thinks the new islet cells are not its own and attempts to destroy them. Immunosuppressant medications may have side effects such as nausea, vomiting, cancer, and infection, which can be mild or serious; however, the medication must be taken every day or the islet cells may stop working properly.
The transplant has risks and benefits which are reflected in the attributes below. We would like you to review these attributes and then answer the twenty treatment option questions in the survey provided to you.
Attribute Table for UCSF Hard-to-Control Type 1 Diabetes PPI Study
PLEASE REFER TO THIS TABLE FOR ANY QUESTIONS YOU MAY HAVE ABOUT WHAT ANY WORDS MEAN WHILE YOU ARE TAKING THE SURVEY
(December 23, 2019)
|
Attribute |
Description |
Levels |
|
Benefits |
||
|
1) Chance of achieving normal range HbA1c (≤ 7.0%) and elimination of severe hypoglycemia by end of Year 1 after final islet infusion procedure |
Clinical treatment success is defined as normal range HbA1c level (e.g., HbA1c ≤ 7.0%) and elimination of severe hypoglycemia. By severe hypoglycemia we mean you have hypoglycemic unawareness and need someone else’s help to get medical attention to treat your low blood glucose level. Those who report frequent severe hypoglycemia have a 3.4 times greater risk of death at 5 years. You may continue to also need insulin in order to achieve your normal range HbA1c after your islet cell transplant. Achieving a normal range HbA1c is important to your overall success in managing your diabetes and means your diabetes is in much better control than when your HbA1c is not in its normal range). Note: The transplant process may involve up to 3 separate infusions over a 3-10-month period to reach clinical treatment success. Treatment success can also require starting or increasing insulin injections. |
i.e. you will see the following image to depict ‘40 out of 100 people’
|
|
2) Duration that normal range HbA1c and elimination of severe hypoglycemia lasts after the final infusion without additional actions |
The length of time clinical treatment success (normal range HbA1c and elimination of severe hypoglycemia) lasts after the final infusion without additional actions. (Your islet cell transplant benefit of reaching your normal range HbA1c can last different amounts of time after your transplant). Remember clinical treatment success is defined as having an HbA1c of less than 7.0% and having no severe hypoglycemic episodes. The duration of clinical treatment success starts after your last of 3 possible separate transplant infusions that may be required to reach success, and could take from 3 to 10 months.
|
i.e. you will see the following image to depict ‘2 years’ |
|
3) Extent of Insulin Independence; need for monitoring sugars, adjusting insulin.
|
Insulin independence means not needing any insulin doses or to monitor sugars or adjust insulin to maintain your blood glucose within the first 5 years after your transplantation. After your transplant you may or may not continue to require insulin. The length of time that you are free of the need for insulin and its monitoring can be not at all, or different periods of time such as:
Insulin independence is defined as freedom from the need to do the daily diabetes maintenance work of monitoring blood sugars and adjusting your insulin. You may have 5 years or less of insulin independence. Some are never independent from the daily need to monitor your blood sugars and adjust your insulin requirements, but you may need less insulin. After 5 years your need for monitoring blood sugars and adjusting insulin is unknown with some studies showing half of the patients remaining off insulin for up to 9 years, with one patient at 13 years. |
|
|
4) Expected reduction in the risk of long term complications |
Having diabetes comes with a risk of certain complications that will occur after a long-time such as developing nerve damage, kidney damage, or eye damage.
It is likely that an islet cell transplant will reduce the risk of these long-term complications, but no one is certain by how much this will be reduced or if the reduction will differ for the different current risks of all type 1 diabetic’s kidneys, nerves in the hands and feet, or retinal eye damage. It may be more important to you to lower the risk of some of these complications than others despite the uncertainty in the amount of reduction.
We will ask you to choose for:
|
|
|
Risks |
||
|
5) Risk of treatable procedure-related Adverse Events |
You may have different amounts of risks for Treatable procedure-related adverse events after your islet cell transplant procedure(s). They are generally treated by giving medications, or taking medicines to prevent them. They would require doctor visits, but not a hospitalization. Some of these treatable adverse events include:
Your risks can range from none to 40%. This means that either none, 5 people out of 100 people, 15 people out of 100 people or 40 people out of 100 people have one of these treatable procedure related adverse events.
|
i.e. you will see the following image to depict ’15 out of 100 people’
|
|
6) Risk of Serious Complications requiring hospital treatment and rare death |
You may have different amounts of risks for Serious Complications requiring hospital treatment after your islet cell transplant procedure. Your risks can range from none to 15 percent. This means that either none, 1 in 100 people, 5 in 100 people or 15 in 100 people have one of these serious complications. They generally require hospitalization for treatment and very rarely they can lead to death. These Serious Complications and their hospital treatments include:
|
i.e. you will see the following image to depict ‘5 out of 100 people’
|
|
7) Restrictions, medicines, monitoring due to risks of life long ‘anti-rejection drugs’ as long as your islet cells are working (up to 5 years or longer) |
‘Anti-rejection drugs’ must be taken as long as islet cells are working. You likely also will take added anti-inflammatory drugs. These medications require restrictions and constant monitoring for prevention of moderate risks. Anti- rejection drugs are taken to block the immune system to protect from rejection of your transplant. They work well but also have limitations that require you to be more careful of certain things, to take some medicines, and to obtain testing to prevent their bad effects. These limitations include:
|
|
|
8) Time and support required if needing multiple transplant infusions (1 to 3), each requiring 3 months |
In order to go through with the islet cell transplant, you will need to dedicate time and support to have the procedure and manage your diabetes. 1 transplant infusion takes up to one week (usually 3-5 days) of hospital stay, 2 weeks of intensive monitoring of blood sugars and insulin need, and monthly physician visits. You would also need the support of another person to help you in the recovery and management process. All inclusive, 1 procedure would take a total of 3 months time and support. There is a chance that you may need to have more than one transplant infusion in order to achieve the desired results. Each additional infusion that you might require will each take an additional 3 months of your time for recovery, and the support of an additional person to help you.
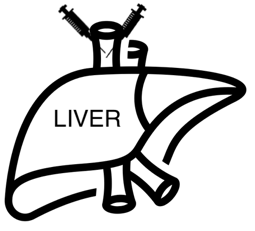
The image of your liver shown on the right shows 2 syringes so means that you will need time and support for 2 islet cell infusions for a total of 6 months of time/support |
i.e. you will see the following image to depict ‘6 months’
|